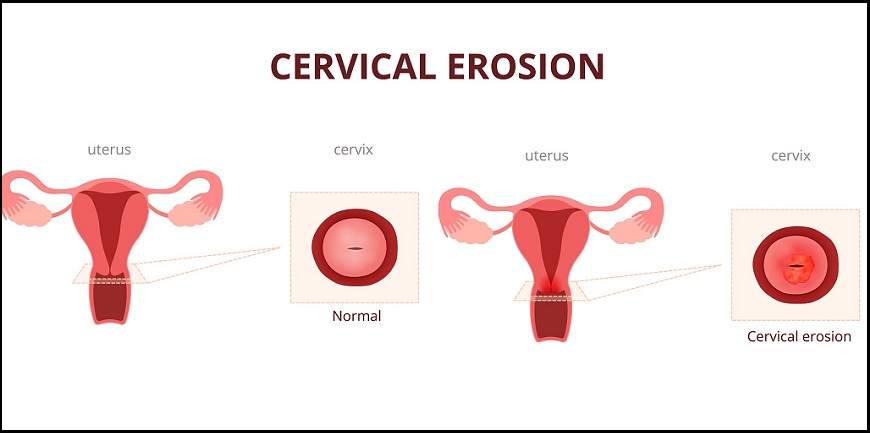
Cervical ectropion, or cervical ectopy, is when the soft cells (glandular cells) that line the inside of the cervical canal spread to the outer surface of your cervix. The outside of your cervix normally has hard cells (epithelial cells).
Where the two types of cells meet is called the transformation zone. The cervix is the “neck” of your uterus, where your uterus connects to your vagina. This condition is sometimes referred to as cervical erosion. That name is not only unsettling, but also misleading. You can rest assured that your cervix isn’t really eroding. Cervical ectropion is fairly common among women of childbearing age. It’s not cancerous and doesn’t affect fertility. In fact, it’s not a disease. Even so, it can cause problems for some women. Read on to learn more about this condition, how it’s diagnosed, and why it doesn’t always require treatment.
What are the symptoms?
If you’re like most women with cervical ectropion, you won’t have any symptoms at all. Oddly enough, you may not be aware you have it until you visit your gynecologist and have a pelvic examination.
If you do have symptoms, they’re likely to include:
Some of these are:
What causes this condition to develop?
It’s not always possible to determine the cause of cervical ectropion. Some women are even born with it. It can also be due to hormonal fluctuations. That’s why it’s common in women of reproductive age. This includes teenagers, pregnant women, and women who use birth control pills or patches that contain estrogen. If you develop cervical ectropion while taking estrogen-containing contraceptives, and symptoms are a problem, ask your doctor if it’s necessary to switch your birth control. Cervical ectropion is rare in postmenopausal women. There’s no link between cervical ectropion and the development of cervical or other cancers. It isn’t known to lead to serious complications or other diseases.
How is it diagnosed?
Cervical ectropion is likely to be discovered during a routine pelvic examination and Pap test. The condition is actually visible during a pelvic exam because your cervix will appear bright red and rougher than normal. And it might bleed a little during the exam. Although there’s no connection between them, early cervical cancer looks a lot like cervical ectropion. The Pap test can help rule out cervical cancer. If you’re not having symptoms, and your Pap test results are normal, you probably don’t need further testing. If you’re having difficult symptoms, such as pain during sex or heavy discharge, your doctor might want to test for an underlying condition. The next step may be a procedure called colposcopy, which can be done in a doctor’s office. It involves powerful lighting and a special magnifying instrument to get a closer look at your cervix. During the same procedure, a small tissue sample can be collected (biopsy) to test for cancerous cells.